Mental health services have been seriously neglected in Indonesia, but emergency responses to the Aceh tsunami and conflict have led to new ways of thinking
Byron Good, Mary-Jo DelVecchio Good, and Jesse Hession Grayman
Natural disasters, bombings, and political violence during the past decade have brought issues of trauma and mental health clearly into Indonesia’s national consciousness. Psychosocial programs and mental health services have been key elements in national and international responses to disaster. However, efforts to develop sustainable services for persons with mental health problems have come face to face with the limitations of the country’s mental health system. Indonesia has among the smallest number of psychiatrists and mental health specialists, as well as psychiatric beds, per population of any country in Southeast Asia, ranking only ahead of Papua New Guinea, Cambodia and Laos.
Physicians and other health professionals who work in general medical services often lack training in how to diagnose and treat mental health problems, and the country lacks community mental health services. As a result, the burden of caring for people with serious mental health problems falls almost exclusively on families. Most persons with severe depression or anxiety disorders, as well as children and youth with mental health problems, are largely untreated.
Despite growing awareness about the importance of mental health among national policymakers, less than one per cent of all health care funds are spent on mental health services, and mental health is not listed as a priority for the country’s network of primary health care centres (puskesmas). Indonesia is not unique; mental health goals remain a glaring omission from the millennium goals, and mental health care remains tragically under-funded in most low and middle income societies. It is striking that in Indonesia the vast majority of persons with even the most severe mental disorders do not receive basic medications, and that the number of persons locked in back rooms or constrained by traditional wooden stocks (pasung) continues to be an embarrassment to the country.
Ironically, some signs of positive change have come out of Indonesia’s worst experiences in recent times. With the violence at the end of the Suharto era, successive bombings in Bali and Jakarta, and momentous natural disasters, including the tsunami in Aceh and numerous earthquakes, ‘trauma’ has entered the national vocabulary, along with the awareness of the importance of providing mental health care to those most severely affected. A number of Indonesian professional networks and specialised NGOs – such as Yayasan Pulih in Jakarta and Yayasan Kanaivasu in Bali – have developed model programs of trauma treatment. Policymakers have become increasingly aware of the importance of such programs.
Though the use of the words ‘stress’ and ‘trauma’ in Indonesian often differs significantly from that in English, these shared words serve to bridge local understandings of the personal effects of violence and disaster and the rising interest of many NGOs and intergovernmental organisations in providing psychosocial and mental health services in response to disaster. Out of this fusion, new approaches for treating mental illnesses have begun to emerge.
The Aceh effect
The province of Aceh has been critically important for the development of new models of mental health care. The Great Indian Ocean Tsunami of 26 December 2004, which had such profound effects on the coastal communities of Aceh, led to one of the greatest outpourings of humanitarian response in history, with more than 300 international organisations and Indonesian NGOs flowing into Aceh. When the Government of Indonesia and the Free Aceh Movement (GAM) signed a peace deal on 15 August 2005, the humanitarian response, already underway, was widened to include post-conflict communities, particularly those up in the hills. Humanitarian organisations recognised the enormous personal and psychological suffering associated with the disaster and the years of conflict. They used the term ‘trauma’ to legitimise the search for funds to provide psychosocial and mental health services to both post-tsunami and post-conflict communities. Aceh thus became a global laboratory for the development of post-disaster and post-conflict psychosocial and mental health responses.
The programs in Aceh had several characteristics. First, they were widely dispersed and enormously varied in the nature of services and populations targeted. Some focused on training, developing short courses for doctors, nurses, and teachers on how to recognise and respond to the effects of traumatic experiences. Other programs provided direct services such as recreational activities, schooling, and play groups for children and youth, particularly those displaced by the tsunami and living in the barracks. Some organisations developed community-based psychosocial programs, focusing on reconciliation among (perceived) conflicting groups in communities or on reintegration of former combatants into their home communities. Others focused explicitly on providing ‘trauma treatment’, via special ‘trauma clinics’ or group therapy programs for villagers in conflict-affected districts. Some programs provided direct services, while ignoring government agencies and even regulations; others closely coordinated with provincial and district offices of the Ministry of Health or led efforts to develop a provincial mental health policy.
While extremely important services were provided, the second over-riding characteristic of these programs was that they were largely undocumented and with few exceptions not formally evaluated. If Aceh was a laboratory, it was one which carried out experiments but did not record results systematically nor provide scientific analysis of what was done or what worked successfully and what did not. Almost no agencies provided genuine accounting of benefits and costs that could be used by policy makers to determine where and how funds should be invested in psychosocial and mental health programs across Aceh and throughout Indonesia. A great opportunity was lost to learn from this experience.
One program with documented success

IOM’s mental health mobile clinic in a village - MaryJo D. Good
Our work with the International Organization for Migration (IOM) was one exception to the general failure to evaluate programs and policies. As part of its role in the administration of the peace process, IOM Indonesia sought funds to provide services not only to former prisoners and combatants, but also to families and communities most affected by the conflict. IOM made the unusual decision to contract with the Department of Global Health and Social Medicine at Harvard Medical School to support the development and evaluation of programs in the area of post-conflict mental health care. This unique arrangement led to an intensive collaboration over five years, which included the design and implementation of a major ‘psychosocial needs assessment’, followed by a pilot intervention program using mobile teams to provide mental health care to 25 highly conflict-affected villages, and later extended to 50 more villages. Formal documentation and evaluation of these services and their outcomes, as well as training and supervision of health care workers and close collaboration with district health offices, was central to this program.
The ‘psychosocial needs assessment’ was designed in late 2005 to help guide the development of the IOM program. Our goal was to evaluate levels of traumatic events associated with the conflict, levels of psychological and psychiatric symptoms, levels of disability associated with mental health conditions, and desire for particular kinds of services. Working with teams from IOM and Aceh’s Syiah Kuala University, surveys were conducted to provide representative data of adults in villages in high conflict subdistricts first in three districts on Aceh’s north coast, then in 11 more districts around Aceh. (On-line copies of the IOM reports that resulted can be found here and here.)
The surveys found shockingly high levels of conflict-related traumatic experiences, particularly in Aceh’s north, east and southwest regions. In those areas, 78-80 per cent of adults experienced combat; 48-66 per cent of men reported being beaten, and 24-25 per cent of men reported being tortured. The surveys also documented extraordinarily high rates of psychological symptoms, comparable to those in war zones such as Bosnia. The survey and associated interviews documented that villagers had a strong desire for mental health services, as well as for other forms of support, but that powerful memories of the surveillance of the health care system by the military were preventing them from seeking treatment.
The challenges of providing mental health services were enormous. Aceh had not only usual forms of mental illnesses (standard epidemiological figures suggest rates of over one per cent of adults with major psychotic illnesses alone – over 20,000 persons in Aceh), but also high levels of mental health problems from the terrible losses associated with the tsunami and years of conflict.
Acehnese are resilient, and many recovered over time without medical forms of mental health care. However, many continued to show signs of classic PTSD – of reliving terrible events they had witnessed or experienced, with associated nightmares, panic attacks, and anxiety – as well as elevated rates of depression, sleep disorders, and disabling anxiety (see ‘No nightmares in Aceh’, Jesse Grayman’s analysis of how trauma was expressed through dreams, based upon this same research). To respond to these problems, Aceh had only four full-time psychiatrists for a population of over 4 million people at the time of the tsunami, one psychiatric hospital, and no psychiatric units in district hospitals. By contrast, Australia, with 13 psychiatrists per 100,000 population, would have approximately 420 psychiatrists for a province of equivalent size, along with community mental health clinics, acute wards, specialised services for children and adolescents, and an even greater number of psychologists, psychiatric nurses, and psychiatric social workers.
Treatment in the villages

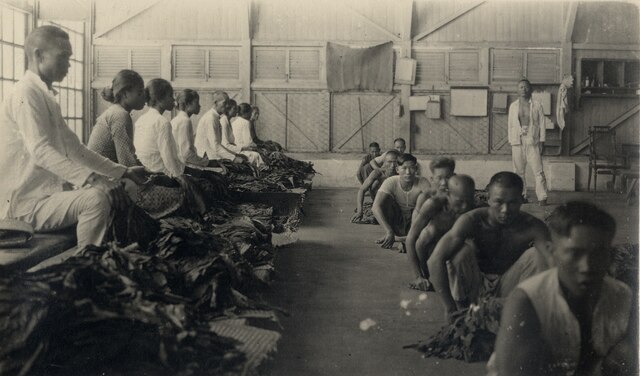
Providing prescribed medications - Jesse H. Grayman
Given these limitations, we worked closely with IOM to develop a model that could provide services to particularly high conflict and relatively isolated villages on an emergency basis, while building capacity within the primary health care system. A small group of dedicated Acehnese general practitioners and nurses were given short, specialised training and close supervision by an Acehnese psychiatrist. They formed mobile mental health outreach teams, who along with nurses from the primary health care centres, went into villages, provided general medical care, sought out persons with mental health problems, and provided treatment – including diagnosis and medication, counseling and family visits, the formation of village level support groups, and in a subset of villages, ‘livelihood’ support. Nearly 2100 people in 75 villages were treated over a period of three years.
The evaluation research provided strong evidence for the benefits of this model of mental health services. First, it demonstrated that competent mental health care could be provided by GPs and nurses making monthly visits to villages, and that such services would be strongly supported by local communities. Teams treated approximately six per cent of village members. Of these, only a small number suffered psychotic illnesses or organic brain disorders; the vast majority were treated for depression, anxiety, and post-trauma mental health problems.
Second, the research demonstrated that overall, rates of recovery were remarkably high, for men and women. Of 1077 persons in the treatment study sample, 83 per cent reported some to great improvement in their symptoms. The per cent of persons with the highest levels of anxiety symptoms dropped from 43 per cent before treatment to 11 per cent after treatment; those with high levels of PTSD symptoms from 26 per cent to eight per cent.
Third, the project demonstrated that common mental health disorders are terribly disabling, and that treatment is extremely powerful in returning individuals to regular work and social functioning. When individuals entered treatment, they reported that before they became ill, they were able to work on average 28 hours per week (even though limited by the conflict); when they fell ill, this was reduced to 10 hours per week. At the end of treatment, individuals reported that they could now work an average 41 hours per week!
The IOM project showed that a model of training and supporting general practitioners and nurses to deliver full-time mental health care, providing them good supervision and access to referral, and using mobile mental health teams is extremely effective for providing services to a population with high levels of mental illnesses in a region with extremely limited mental health resources – and virtually no psychiatrists. This model of care, however, requires financial and administrative support beyond what Indonesia currently invests in mental health.
At the same time, the IOM project was like many other psychosocial and mental health projects developed by humanitarian organisations. It was focused on responding to an acute situation, not on the long-term. By 2010 IOM, along with nearly all other organisations, had stopped supporting mental health programs in Aceh. The international community provided critical services in the four or five years following the tsunami and the peace deal. Important investments were made in rebuilding hospitals and primary health care centres, critical services were provided, and many professionals were trained in trauma-related mental health problems.
However, nearly all humanitarian agencies worked with an ‘exit strategy’ in mind, which included phasing out funding, developing ‘sustainability’ plans, and turning services over to local government and non-government agencies. While these plans sounded promising on paper, ‘sustainability’ was most often little more than a slogan.
A model for the future?

Patient recovery leads to revitalised household economies - MaryJo D. Good
What has developed by 2013? Despite the problems outlined above, the post-tsunami and post-conflict programs in Aceh left important legacies. A number of young Acehnese physicians have gone on to advanced training in psychiatry and returned to practice in local communities. Today there are 16 psychiatrists working in the province: still a tiny number for a population of over 4 million, but a major improvement nonetheless. Several district hospitals have developed psychiatric services, meaning families of acute patients no longer have to take them to Banda Aceh. Nurses in many primary health care centres have received basic training as community mental health nurses, and spend part of their time traveling to villages to provide basic care for those with the most severe mental illnesses.
Aceh’s previous governor, Irwandi Yusuf, launched a ‘bebas pasung’ (stock free) program, which supported identifying individuals in physical constraints and bringing them to the hospital in Banda Aceh for free treatment, before returning them home. In addition, young, activist physicians, including psychiatrists, are developing small but important programs of community-based care and rehabilitation services in specific, local communities.
A broad model has evolved as government policy in Aceh – in part growing out of meetings of stakeholders organised during the post-tsunami period. In this model, the primary health care centres (puskesmas) should be the centre of mental health care. GPs in these centres should receive mental health training and administer medications, and each centre should have several trained specialist mental health nurses who provide outreach care.
In the villages, where families remain the primary unit of mental health care, specialised village cadres – volunteer health workers – should be trained to link those with mental illness and their families to the puskesmas. Referrals should go upward to a psychiatric unit in district hospitals, staffed by a psychiatrist, and these should refer upward to the provincial mental health hospital.
This broad model expands well beyond the old model, inherited from Dutch colonial times, that focused exclusively on building and staffing provincial psychiatric hospitals for those with chronic psychotic illnesses. It is emerging as a de facto policy of what may one day constitute an integrated mental health system in Indonesia. However, the model is not far advanced in implementation. Most community mental health nurses, where they exist, have only been provided basic courses, while the work they are expected to do requires more advanced training. Physicians cycle through the primary health care system, and new physicians are often not provided mental health training. Funds for mental health care remain woefully inadequate.
The politics of mental health are too often a politics of neglect. Activists, journalists and the general public often give their attention to the politics of commission. The politics of structural violence and omission – of the neglect of the human rights of those with highly treatable mental illnesses – are, however, often as devastating as acts of overt violence. Unfortunately, such politics are global. Thankfully, there are at least signs now in Indonesia of the beginnings of a realistic model for mental health care, one that respects the human rights of people with mental illness and provides competent and humane services for those in need. We should not be unrealistic about what has been achieved, but there is a growing space for hope and optimism.
Byron Good (byron_good@hms.harvard.edu) is a professor of medical anthropology and Mary-Jo DelVecchio Good (maryjo_good@hms.harvard.edu) is a professor of social medicine, both at Harvard Medical School. Jesse Hession Grayman (jgrayman@gmail.com) recently completed his PhD in the Department of Anthropology at the Harvard Graduate School of Arts and Sciences.