Abolishing Indonesia's practice of physically restraining the mentally ill has some way to go
Versi Bh. Indonesia
Abolishing Indonesia's practice of physically restraining the mentally ill has some way to go
Irmansyah
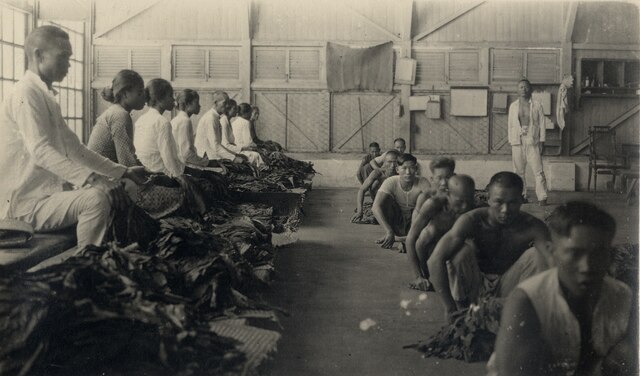
Pasung is the practice of restraining people – particularly individuals with severe mental illness – using wooden blocks and chains, or confining them in a small room, in order to limit their freedom of movement. Unfortunately, the practice is still common in Indonesia, especially in rural and remote areas.
In October 2010, the Ministry of Health initiated the national program ‘Indonesia Bebas Pasung’ (Indonesia Free from Pasung) and asked all sectors of government to commit to working with local communities to eradicate the practice. Indonesia faces many mental health problems, but the ministry chose to focus on pasung for several reasons. Most importantly, the practice is utterly inhumane and involves almost all members of a community – it is impossible to imagine a worse experience for people with mental illness. Second, its occurrence demonstrates the mental health system has malfunctioned. In attempting to eradicate pasung, the ministry hoped to improve Indonesia’s mental health care system as well.
A decade has now passed since Indonesia Bebas Pasung began. It is timely to reflect on what has been achieved so far.
There certainly have been some improvements in specific localities and with respect to certain issues. Compared to 10 years ago, mental disorders are no longer as stigmatised. Consumer organisations have also been established and now cover almost all mental health issues. There are groups that address specific disorders, such as the Indonesian Schizophrenia Support Community and Bipolar Care Indonesia. Other groups focus on education and advocacy, such as the Indonesian Mental Health Association, Pulih Foundation (which focuses on providing psychological services to victims of violence and natural disasters) and Into The Light Indonesia (which focuses on suicide prevention). These associations play an important role in increasing general awareness of mental health issues. They also advocate for improvements in the mental health care system and for better mental health policy. These groups are not only active in Jakarta, but in remote areas as well.
Today, the Indonesian government pays more attention to mental health issues than it did before; multiple ministries are part of the effort. The Ministry of Social Welfare has made Indonesia Bebas Pasung a priority. The Ministry of Law and Human Rights has released a special report on mental health issues, which recommended the government take the lead in improving the mental health care system. The Ministry of Manpower is paying attention to mental health issues in the workplace, and the National Commission on Human Rights has initiated an advocacy movement to protect the rights of individuals with mental illness. These developments all contributed to the passing of the Mental Health Law in 2014, a powerful tool for improving mental health in Indonesia.

The implementation of a new universal health insurance system in 2014, and the ensuing requirement of accreditation for all health facilities, has increased the accessibility of all health services and improved their quality. People with mental illness and their families have benefited, particularly in hospitals where they receive better services and medication, and no longer have to worry about costs. For better mental health at the community level, however, improved policies and hospital services alone are not enough. Additional large-scale national programs are needed.
Community health success
Indonesia’s national ‘Promoting a Healthy Paradigm’ initiative comprises two major health programs: the PIS-PK (Healthy Indonesia through a Family Approach Program) and GERMAS (a community campaign to promote healthy living). Mental health is a focus in both programs. PIS-PK, launched in 2017, mandates that each community health centre visit all families within its coverage area to evaluate their health status using 12 indicators. These indicators include family planning, antenatal care, immunisation, breastfeeding, child growth monitoring, tuberculosis, hypertension, mental disorders, smoking and health insurance, as well as access to clean water and sanitation. GERMAS encourages individuals to check their health regularly, eat healthy food, be physically active, quit smoking, have enough rest, and manage stress well. Mental health is an intrinsic part of both programs, and both programs are applied on a large scale.
The PIS-PK program in particular has had a positive influence on mental health. In the past, community health centres usually served the community via health posts or integrated service posts, a monthly neighbourhood or village health post run by volunteers that focuses on maternal and child health. Staff from the community health centres visit these health posts and examine everybody who attends. However, because many individuals never visit these posts, the health centre does not know anything about the health status of the community as a whole. Now, through the PIS-PK program, health centres are mandated to visit all families in their catchment area and submit their findings to a Ministry of Health database. This reporting system enables the ministry to monitor nationwide data, resulting in a better understanding of mental health at the national, district and sub-district levels. We are beginning to see some modest improvements.
When PIS-PK was first implemented, the scores on the mental health indicator were discouraging; they remained at the bottom of the list of all health indicators. Only about 10 per cent of individuals with mental health conditions received appropriate treatment, whereas approximately 90 per cent either received insufficient treatment or received no treatment at all. The first concrete data on the state of the nation’s health shocked officials and encouraged them to look for ways to improve the indicators. They used the PIS-PK data to identify individuals with untreated mental disorders and ensured they received treatment. The effects soon became clear, and improvements in the scores of overall family health were discernible. The latest data is encouraging: the mental health indicator is currently at around 26 per cent and has moved from the twelfth to tenth position. The PIS-PK and GERMAS programs have increased awareness of mental health and made the occurrence of mental health problems in society more visible. In addition, mental health is now more commonly understood to be a key responsibility of community health centres.

The PIS-PK program currently reaches more than 47 million family households – about 72 per cent of all families in Indonesia. This means that 72 per cent of individuals with mental illness who live with their family have now been identified. Ideally, community health centres must provide services to individuals with mental disorders. Most health professionals are aware of this by now, but, unfortunately, not all primary health centres are capable, or sufficiently confident, of providing treatment to individuals with mental health problems. There are two major barriers: the availability of medication as well as human resources.
Future action needed
The 2014 Mental Health Law and other health policies, as well as the general improvement of mental health services, have contributed to making mental health a key point on the national health agenda. Unfortunately, more and better policies are not sufficient to provide mental health services to the whole population, especially at the community level. Data from RISKESDAS (the Basic Health Survey) shows a slight improvement in mental health at the community level. In particular, the data on pasung – individuals with mental illness who have experienced pasung at least once during their lifetime – indicates a slight decrease, from 14.4 per cent (2013) to 14 per cent (2018). The data from 2018 indicates that about 30 per cent of these individuals had been subject to pasung within the last three months.
Under the ‘Promoting a Healthy Paradigm’ initiative, progress has been made: there have been improvements in the awareness of mental health and mental health literacy has increased. This provides a good foundation for better mental health services. The objective should now be to implement all policies and deploy all mental health resources at the community level to improve the quantity and quality of mental health services. Additional large-scale programs are needed, including programs to improve the availability of human resources in mental health. This can be achieved by providing additional training for health professionals. Unfortunately, a school for mental health nursing was closed many years ago, but it could be opened again and fulfil the need for community mental health nurses in primary care. Professional social workers and occupational therapists, who currently are only minimally involved in mental health care, should be encouraged to participate in providing mental health services. Making medications available to community health centres is very important as well.
Irmansyah (irmansyah@gmail.com) is associated with the Indonesian National Institute of Health Research and Development, part of the Ministry of Health.