Indonesia’s Mental Health Law will have little impact without more regulatory support
Versi Bh. Indonesia
Indonesia’s Mental Health Law will have little impact without more regulatory support
Nova Riyanti Yusuf
The specialist psychiatry training I received at Universitas Indonesia was a crucial moment in my life. It was then and there that I witnessed the real conditions of individuals with mental health problems in Indonesia – both by seeing patients, and by hearing caregivers’ cries for help. Around that time, I also became aware of how the international media reported on the condition of mental health services in Indonesia: it was characterised as among the worst in Asia.
I quickly became tired of trying to change things from within the medical system. I wanted to avoid becoming a disillusioned medical practitioner who only treats symptoms. I became determined to address the root of the problem. I realised that, for me, making a real difference meant embarking on a very different career; that whether I liked it or not I would need to roll up my sleeves, get into politics, and try to change things from the centre of power.
I was not sure how to go about this, but then I unexpectedly received an offer to enter the political arena. In 2005, I had already accepted an invitation to become a member of the Democratic Party, the ruling party from 2004 to 2014. After much hesitation, I accepted their invitation to run for parliament in the 2009 elections. I heeded the advice of a fellow psychiatrist who warned me not to go crazy if I was not elected. It is public knowledge, yet also something that is difficult to admit, that if one enters the world of politics, one tries to reach a powerful position. And that the disappointment can be crushing if one does not succeed.

The same year that I graduated as a psychiatrist I was elected to the House of Representatives (DRP) for 2009 to 2014 by the DKI II constituency, which consists of South Jakarta, Central Jakarta and Indonesian citizens living overseas. I won the second-highest number of votes. The same year that I entered office, I initiated what later became known as the Mental Health Bill at the commission I was assigned to by my faction, known as ‘Commission IX’. We oversaw health, manpower and transmigration, food and drugs, family planning, and population affairs.
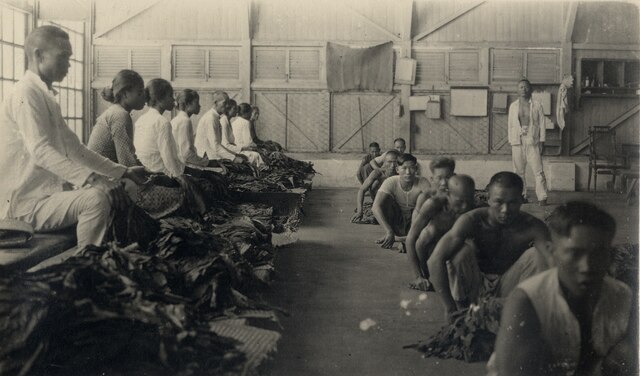
Delivering the bill
In 2009, as an eager but new and inexperienced member of parliament, I initiated the Mental Health Bill and successfully delivered it into the National Legislation Program for 2010 to 2014. I was driven by a desire to deliver justice to the 18,000 individuals with mental disorders whose human rights were being violated by being caged, shackled, locked up and/or physically restrained by their families, communities or the shelters in which they were institutionalised. Initiating a bill is, however, only the first step. I needed an enormous amount of persistence and willpower for what followed. A bill can indeed change lives, but to get it passed one needs to know the long and winding road of Indonesian politics.
In my role as a legislator, the Health Commission encouraged me to increase the allocated budget for mental health within the Ministry of Health from Rp.9.5 billion in 2009 to Rp.45 billion in 2012 (roughly, from A$1.2 million to A$4.5 million). This increase was still not a large portion of the national health budget, but we took whatever funding the minister would give us.
In 2010 there was a heart-breaking series of suicides by individuals who jumped off high-rise buildings. At that time, I questioned a plan to eliminate the Directorate of Mental Health in the Ministry of Health. As a result, not only did the minister cancel the proposed elimination, she initiated a hotline service (500-545) for psychosocial assistance. It was a good initiative, albeit with many flaws. The hotline eventually disappeared under the guise of an upgrade. It was only reinstated recently.

To ensure that the Mental Health Bill remained a priority for the Health Commission, I had to initiate some model projects to demonstrate that the law would not only be of sentimental value. I had to provide evidence-based examples of best practice in mental health care. One of the model projects I developed was a Mobile Mental Health Service. It functioned both as an outreach service and as a promotional effort in urban areas, and could also be used as a psychological first aid facility in areas affected by natural disasters.
To make a long story short, it took the support of the entire universe to help me get through all the steps. Afterwards, a prominent national book publisher asked me to write about my experiences as a politician, so I wrote A Rookie & the Passage of the Mental Health Law: The Indonesian Story (Gramedia, 2014).
With the support of fellow legislators and expert staff, I managed to get the bill passed into law on 18 July 2014. This moment, five years after I initiated the process, felt like a triumph. Staff from the Ministry of Health and several people with mental disorders joined me for a celebration in the fountain in front of the parliamentary complex. We were so relieved that the bill had been approved and codified into law.
That jump into the fountain, however, turned out to be a bittersweet moment. It made me, in the eyes of some, one of the coolest MPs ever, but one person accused me of simply seeking attention, and has forbidden me from sharing the contents of an email he sent me on the matter. I still suffer from the insinuation that this celebration was just a brazen attempt to get media exposure for myself rather than to highlight the work and suffering of many others.
The law
What is the Mental Health Law, or Law No.18/2014, all about? The law is obviously inspired by the new spirit for policy reform, social inclusion, the fight against stigma and discrimination, and the upholding of human rights. It is an ambitious document with 10 chapters that cover everything from general provisions to the establishment of a National Institute of Mental Health. The general provisions provide definitions that, among other things, distinguish between individuals with mental health problems (orang dengan masalah kejiwaan, or ODMK) and individuals with mental disorders (orang dengan gangguan jiwa, or ODGJ). This terminology is now widely used to destigmatise individuals who have previously been called ‘crazy’.

My efforts to destigmatise mental illness and mental disorders were meant to ease the everyday lives of individuals and remove limits placed on their educational and employment opportunities. They also face obstacles when accessing health care. The stigmatisation is clearly visible in news reports, in the mass media, and on social media. Stigma and discrimination are also evident in how individuals with mental disorders are frequently restrained or treated violently.
The Mental Health Law mandates the creation of a mental health care system that includes four elements: health promotion, preventive care, treatment and rehabilitation. The law prioritises both promotive and preventive efforts. Promotive efforts are undertaken in various environments including via the mass media. Preventive efforts are implemented primarily within family settings. Equally important are rehabilitative efforts, which prepare individuals with a mental disorder to become full and active members of the community. Of key importance are a number of prohibitions, especially directed at health workers, which ban any form of violence against individuals with mental disorders or restraining them in any way.
Further provisions state that mental health efforts should be integrated, comprehensive and sustainable. This has since been mandated by a presidential regulation (a perpres) but more such support is needed to strengthen the Mental Health Law. Like any other law, it requires regulations to be issued at the ministerial level to provide clear and practical guidelines on how the principles of the law should be implemented. At the same time, sufficient budget must be made available to cover the expenses associated with the implementation of the law. All such supporting regulations are meant to be issued no later than one year from the enactment of a law, which means that in this case this should have taken place in 2015. It is now 2020 and still no regulations other than that one perpres have formally been issued.
A bitter moment of realisation
After finishing my first round of service in Indonesia’s parliament and seeing the Mental Health Law passed, I found out how difficult it is to implement a law. This is deeply frustrating, yet I keep trying to maintain a sense of urgency among all stakeholders for the establishment of a National Institute of Mental Health. Sandiago Uno, whom I met at a television talk show in 2007, was elected deputy governor of Jakarta in 2017. During his election campaign I was able to brief him on our mandate to establish the Indonesian equivalent of the American National Institute of Mental Health. He was very supportive and requested that I develop a concept plan with his staff. We had been working on it for almost six months when he suddenly announced his candidacy for vice president in the national elections the following year. My hopes, once again, were shattered. Without his leadership it seemed that this project would never go anywhere.

After numerous failed attempts, I have begun to accept that the Mental Health Law will never be formalised into practical regulations supported by associated budgets. And this is despite the fact that Indonesia has the fourth-largest population in the world and that the country faces many mental health problems, including an increasing number of suicides. The country also carries the mental health burden of many natural disasters and, of course, of the Covid-19 pandemic. This problem was also acknowledged by the United Nations on 14 May 2020, when it issued a call to protect the most vulnerable people from mental health issues during and after the pandemic. Decades of neglect and under-investment in addressing people’s mental health needs have been exposed by this crisis. A key part of the UN appeal is to include mental health care in all government Covid-19 strategies, which is particularly important because the average national expenditure on mental health is just two per cent – not of total national expenditure, but of the national health budget.
The UN call really underscores our national problem when it comes to prioritising mental health needs. Indonesia, again, did not include mental health in its most recent national mid-term development plans. And suicide prevention has again not been included in our national blueprints for achieving the World Health Organisation’s Sustainable Development Goals.
I honestly do not know what else to do, but I will keep going and, like all of us, try to preserve my own mental health during this pandemic. The journey of the Mental Health Law is not a great topic to reminisce about during the pandemic. Perhaps I should stop right here. Let us hope for a miracle, shall we?
Nova Riyanti Yusuf (noriyu.md@gmail.com) is a psychiatrist, the initiator of the 2014 Mental Health Law, a former member of the House of Representatives, and the secretary general for the Asian Federation of Psychiatric Associations.