An international team of researchers charts a course for change
An international team of researchers charts a course for change
Byron J. Good, M. A. Subandi, Carla Raymondalexas Marchira, Fiddina Mediola, Tri Hayuning Tyas, Sandeep Nanwani, Ariana Marastuti, & Mary-Jo DelVecchio Good
In 2013, in an issue of Inside Indonesia dedicated to Aceh, the senior authors of this paper described the development of mental health services in post-tsunami, post-conflict Aceh and asked whether Aceh would provide ‘A new model for mental health care?’ for all of Indonesia. Here we return to this question, but now in the context of years of research in Yogyakarta. We ask specifically whether community-based, recovery-oriented models of mental health care can be brought to scale for Indonesia.
Over the past decade, the authors of this paper have come together as a mental health working group, linking the Faculty of Psychology and the Department of Psychiatry at Gadjah Mada University (UGM) with the Department of Global Health and Social Medicine at Harvard Medical School. The group is committed to conducting ‘action research’ aimed at strengthening mental health care, especially for people living with psychotic illnesses.
A standard of care
Since 2016, this work has responded explicitly to a new mandate that district governments should be responsible for the care of people with severe mental illness. The national government has a list of Standard Minimal Services (SPM - Standar Pelayanan Minimal), which district governments are responsible for providing to their citizens. Districts are required to give account of the provision of these services, and evidence of compliance with each SPM is required for accreditation of health care institutions.

This new mandate provides a special opportunity for universities and NGOs to work with District and Provincial governments to develop evidence-based models of care that are feasible for extending throughout the public health system. But what kind of system of care, and how can such services be implemented in all districts in the way that vaccinations or maternal-child care are routinely carried out in in community health care (CHC) centres or puskesmas throughout the country?
This requires building an integrated system, from puskesmas to village kader (village health volunteers), and through referral to district hospitals and psychiatric facilities, all supported by district and provincial health offices. Implementing such a system requires, for example, specific protocols for each type of health care worker linked to types of problems (for example, acute onset of psychosis, pasung or locking, access to medicines and insurance, problems of compliance or relapse).
Our team has asked throughout this work what the overall goal of such care should be. Access to services for all who suffer an acute psychosis? Absolutely. Continuity of care with access to medications over time? Absolutely. But should the overall goal be to enable persons with severe mental illness to recover? What does recovery mean in this context? And what would a ‘recovery-oriented mental health care system’ look like in a setting with low levels of mental health resources? These are more difficult questions, not only in Indonesia but globally.
A need for integrated services
Over the past decade, our team has focused on both of these issues. By working directly with the public health sector, with support from USAID and the Harvard Center for Global Health Delivery-Dubai, we have learned that there is no genuine integrated system of mental health services at the district or provincial level, even in a province like Yogyakarta. There are examples of PHC centres that provide outstanding mental health care and deserve to be models for the country. But there is enormous variation across puskesmas. In one study of five CHC centres, our team found that the number of persons with schizophrenia registered with the puskesmas ranged from 1.4 cases to 15.4 cases per thousand members of the population. Our study of 22 PHC centres in one Yogyakarta district found major differences in anti-psychotic medications available across puskesmas, and similarly in levels of mental health training for GPs and programer jiwa, the heads of mental health programs in the puskesmas. We found that routine monitoring of patients treated for severe mental illness – for symptoms, side effects of medications, and social functioning – were almost entirely absent. In earlier work, our team found that mental hospitals have very limited ‘discharge planning’, leading to poor communications between provincial hospitals and PHC centres after discharge from treatment.

The lack of a continuous, integrated system of mental health care has serious consequences. One of the studies undertaken by our team evaluated an important bebas pasung or ‘unlocking’ program in the Soerojo Mental Hospital in Magelang to learn what happened to individuals who were unlocked, treated in the hospital, and returned home. The study found that families strongly valued the program, but that 21 per cent of the 63 individuals in the sample studied had been re-locked during the two years following hospitalisation. (This contrasted with a Chinese program that showed 8 per cent relocked after 7 years.) The primary concern expressed by families was the lack of follow-up care after the individual was returned home. Simply unlocking individuals, treating them, often quite successfully, then sending them home without genuinely changing the system of care will not lead to good outcomes for those individuals in the long-term.
Our team has worked collaboratively with district and provincial health offices in Yogyakarta, as well as hospitals and CHC centres, to develop an improved system of mental health services to provide care for people with severe mental illness. This has included conducting studies of ‘baseline’ conditions of services, carrying out ‘action research’ projects to respond to particular challenges (such as discharge from hospitals), and collaborating in the development of protocols (often described in Indonesia as ‘SOPs’ – Standard Operating Procedures) for each level of staff in response to specific problems. Developing ‘indicators’ – for services provided, individuals treated, and outcomes – allows reportable findings and the development of targets for improving care.
Moving towards recovery
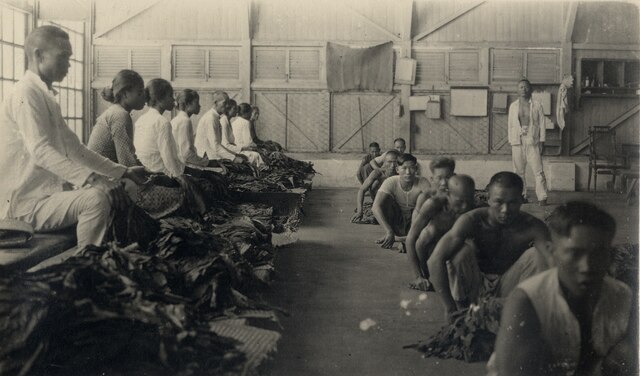
As our team carried out these projects, the question of underlying philosophy of care became more salient. Historically, psychiatry has been pessimistic about the potential for recovery for persons with severe mental illnesses, particularly schizophrenia. Colonial theories of degeneracy, of particular families or groups degenerating genetically, shaped notions of the inevitable decline of those living with a psychotic illness. If it is assumed that people living with severe mental illness will decline throughout their life, it is not unreasonable to provide long-term care. While this assumption led to large, classic asylums, the development of anti-psychotic medications in the 1950s allowed people to be cared for in communities, rather than in long-term living facilities. However, too often even community mental health systems focused primarily on providing sedating medications and continued to assume chronicity is inevitable.
The late 1980s and 1990s saw the emergence of a ‘recovery movement,’ led by those with lived experience of mental illness (‘consumers,’ ‘survivors’) and mental health reformers. Epidemiological studies showed that while psychotic illness often has long-term effects, a decline in functioning over time is often caused more by confinement, neglect, and poor treatment than by the illness. Over a lifetime, approximately 60 per cent of people with a diagnosis of schizophrenia recover fully or in large measure, often eventually living without medications. New medications have had a dramatic effect for some and reduced side effects for others. But recognition that recovery is common played an important role in the development of a new paradigm of mental health care – one that is dedicated to supporting recovery.

What would it mean, then, we ask, if Indonesia were to build not only a more integrated, continuous system of mental health services, but a system oriented toward recovery. Part of the answers are clear. Competent medical evaluation and the best possible medications need to be made readily available. Families and those living with mental illness need to have information about their illnesses and medications. But drugs and education are not enough. Community-based rehabilitation, linking health and social welfare staff in local communities rather than primarily in panti rehabilitasi, are crucial. Village kader need to be trained and given specific roles in such a system. Assessment and services need to be focused on strengths and capacities, not only on symptoms and disabilities.
Our group has explored, for example, the possibility of requiring a ‘recovery plan’ for each individual living with a severe mental illness, rather than simply a diagnosis and prescription. Families providing care need recognition and support, including financial support, since mental illnesses are a common cause of impoverishment. ‘Family gatherings’ have proven effective in giving hope and support to families burdened with providing care. More formal peer and family groups – the Indonesian Schizophrenia Care Community (Komunitas Peduli Skizofreni Indonesia), Bipolar Care Indonesia – are playing an increasing role. Doctors and nurses in puskesmas need to have access to routine support and supervision from psychiatrists, perhaps using telemedicine technologies. Clinical psychologists need to be integrated into PHC centres and given specific roles in such a program. Developing school-based mental health programs, on the one hand, and specialised, youth-friendly, early intervention clinical services for persons in early phases of illness are critical for such agenda. And all of these need to be integrated into routine care.
Hope
This is no modest vision for a nation that has among the lowest number of mental health specialists in Southeast Asia and dedicates only about one per cent of its national health budget to mental health care. But there are reasons to hope that such a model can be developed and implemented in the Indonesian context. While stigma is important in Indonesia, local ideas of recovery – bangkit, pemulihan – are common and provide hope, as Professor Subandi, professor of psychology at Gadjah Mada University, has shown in his research. Psychiatry residents are often eager to be involved in community work, and culturally appropriate models of psychoeducation can be implemented by puskesmas staff, as has been shown by Dr Carla Marchira – the head of the Department of Psychiatry at Gadjah Mada University Medical School.
Indonesian families have strong values of patience and care, and communities, NGOs, and religious groups form strong bases for socially supportive care. Linking universities to public services has great potential for building, evaluating, and formalising new models of care, and an increasing number of young staff in the university are attracted to such a vision. At this moment, national policies that are increasingly supportive of mental health care provide a significant window of opportunity.
It is our conviction that models of community-based, recovery-oriented mental health services can be developed for Indonesia, and that these can be adapted and brought to scale to support those living with mental illnesses and their families. It is this vision that has motivated the work carried out by ‘the Yogya mental health gang’ over these years.
Byron J. Good (byron_good@hms.harvard.edu) is professor of medical anthropology in the Department of Global Health and Social Medicine at the Harvard Medical School and in Harvard’s Department of Anthropology. M.A. Subandi (subandi@ugm.ac.id) is professor at the Faculty of Psychology at the University of Gadjah Mada. Carla Raymondalexas Marchira (cmarchira@ugm.ac.id) is head of the Department of Psychiatry in the Faculty of Medicine at the University of Gadjah Mada. Fiddina Mediola (mediola.fiddina@googlemail.com) is a psychiatrist and head of the Puri Nirmala Mental Hospital in Yogyakarta. Tri Hayuning Tyas (t.h.tyas@ugm.ac.id) is a clinical psychologist and lecturer at the Faculty of Psychology at the University of Gadjah Mada. Sandeep Nanwani (nanwani91@gmail.com) is a physician and program officer for the Adolescent Sexual and Reproductive Health initiative of the United Nations Population Fund. Ariana Marastuti (amarastuti@ugm.ac.id) is head of the Division Community Development at the Center for Public Mental Health, Faculty of Psychology, University of Gadjah Mada. Mary-Jo DelVecchio Good (maryjo_good@hms.harvard.edu) is emeritus professor of Global Health and Social Medicine at the Department of Global Health and Social Medicine at the Harvard Medical School.